INTRODUCTION
In the United States, diabetes remains a pervasive health concern, with an estimated 38.4 million diagnosed and undiagnosed adults affected.1,2 By 2030, it is projected that 16.2% of Detroit’s population will have diabetes, being the fourth highest in the nation.3 The Diabetes Education and Wellness Clinic (DEW), a student-run free clinic, was created to address this long-standing issue by providing resources for those with diabetes in Detroit. Unlike traditional medical clinics, DEW Clinic adopts an interdisciplinary approach and focuses on teaching students and patients alike.
The primary goal of the DEW Clinic is to support patients in learning about their diabetes and assisting them in managing this condition using a Chronic Care Model. The clinic primarily focused on patients with Type II diabetes. Under this model, patients can collaborate with various disciplines - Medicine, Pharmacy, Dietetics, Physical Therapy, Occupational Therapy, Social Work, Law, and Public Health - to develop tailored care plans that fulfill their individual needs and empower them to take control of their health. The secondary goal of the clinic is to provide students with exposure to an interdisciplinary healthcare setting that mirrors the realities of healthcare practices today. As these graduate students prepare for their future healthcare professions, DEW Clinic can offer an invaluable training ground to help them put patient-centered values and interdisciplinary care into practice.
Over the past 4 years, DEW Clinic has successfully supported patients through both telehealth (2020-2022) and in-person clinics (2022-2024), all designed using the framework of a Chronic Care Model. To assess the performance of DEW Clinic, a series of three studies were conducted in the clinic between 2021-2024, examining patient, student, and faculty perspectives on the DEW Clinic model. These studies allowed clinic participants – students, faculty, and patients alike - an opportunity to evaluate the unique structure of DEW Clinic and document their interdisciplinary experiences. The data they contributed served as a basis for students and faculty to make evidence-based decisions regarding the DEW Clinic in the future.
BACKGROUND
The Diabetes Education Wellness (DEW) Clinic was founded in 2009, in response to an overwhelming diabetes epidemic being faced by Detroit’s underserved, underinsured population. Originally proposed by a team of Occupational Therapy graduate students at the Institution, DEW Clinic grew over the next 15 years to include graduate students and faculty from programs across Wayne State University, including Medicine, Pharmacy, Dietetics, Physical Therapy, Social Work, Law, and Public Health. These disciplines work together with the goal of providing personalized care and education to diabetic patients, as well as clinical experience for students preparing to enter the healthcare field. The medical student would predominantly be in their first two years of training to obtain more clinical exposure, while the other disciplines had students in all phases of their training. Each discipline would have a supervising faculty member in the room, observing the patient interaction and ensuring appropriate and adequate care. Since its conception, DEW Clinic has been overseen by multiple generations of students, and has been supported by many faculty members, community mentors, industry benefactors, and other sponsors. While there is no requirement for students to volunteer on a consistent basis, many students come back to the clinic for further exposure.
The clinic’s structure and location has also evolved over time to meet the needs of patients. The DEW Clinic was initially housed within S.A.Y. Detroit Clinic in Highland Park, Michigan, where it offered diabetes care and support for the patients in the Detroit community for the next decade. In light of the COVID-19 pandemic restrictions, DEW Clinic transitioned from a traditional in-person model to a telehealth structure in 2020. To maintain DEW Clinic’s interprofessional framework, each telehealth visit comprised of patient assessments completed by students from seven graduate disciplines: Medicine, Pharmacy, Dietetics, Physical Therapy, Occupational Therapy, Social Work, and Law. Clinics took place once per month over Zoom, with all participants (including patients) participating from their respective homes. During these Zoom sessions, patients spent approximately 60-90 minutes moving through a series of discipline-specific “Zoom Rooms.” In these virtual breakout rooms, representatives from each discipline spoke with a patient about the aspects of diabetic care aligned with their specialty. These discussions were informed by a comprehensive diabetes history provided by the patient in an intake form, which was completed prior to their visit. Following their patient encounter, each discipline held 15-minute focus groups for their students and faculty to discuss the case and high-yield takeaways, and consolidated their recommendations for the patient’s care plan. Telehealth clinic sessions were concluded with an interdisciplinary discussion amongst all students and faculty; these dialogues were focused on summarizing the overall patient case and comparing discipline-specific perspectives. The benefits and challenges of this telehealth model were assessed through a retrospective study conducted by the DEW student executive board in 2021.
In 2022, DEW Clinic transitioned back to an in-person model, held once per month in an Institution-affiliated clinic in midtown Detroit. Graduate students from a broad range of DEW Clinic disciplines joined as volunteers in the clinic in accordance with their academic schedules. Although academic schedules were occasionally asynchronous among these graduate disciplines, at least 3-4 disciplines were represented at DEW Clinic each month to preserve an interdisciplinary model of care. Also in 2022, Public Health joined as the 8th DEW discipline. Upon the patients’ arrival at the clinic, the patient was placed in a private examination room, which was visited by students and faculty representing Medicine and Pharmacy. These representatives took the patient’s vitals (i.e. height, weight, blood pressure) and a detailed health history, guided by an intake form completed by the patient prior to the visit. This intake form included information about the patient’s past medical history, diabetes history, and medication list. History-taking was followed by an evaluation by Pharmacy students, who reviewed the medication list with the patient. The patient was then guided through a series of exam rooms, each of which included representatives from two to three disciplines to optimize the interdisciplinary approach. To promote an efficient clinic workflow, each discipline was assigned specific roles and responsibilities for their patient encounter, as outlined in Table 1. Following the patient’s departure, all disciplines participated in a clinic debrief to discuss key points of the patient case and summarize their recommendations. These recommendations were provided to the patient in an email following their visit. The experiences of patients in this updated in-person model were assessed through a study conducted by the DEW student executive board in 2022.
In 2023, DEW Clinic continued to operate under an in-person model, with involvement from the following disciplines: Medicine, Pharmacy, Dietetics, Physical Therapy, Occupational Therapy, and Social Work. The in-person model was largely preserved, with some changes made to clinic workflow to increase opportunities for interdisciplinary collaboration. One such change was the creation of a “Clinic Navigator” role, which was taken on by one DEW Clinic volunteer at each monthly clinic. While DEW Clinic participants from each discipline remained separated within a series of exam rooms in the clinic, the Clinic Navigator accompanied each patient from room to room. Before each room encounter started, the Clinic Navigator presented any pertinent information to the clinic participants from the discipline, helping facilitate interprofessional communication and collaboration.
Below is a table of responsibilities for each of the disciplines of the DEW clinic. Many of the roles and responsibilities of the disciplines overlapped, and many disciplines would be in the same room, engaging and observing the patient interaction simultaneously. Furthermore, while other discipline services like podiatry and ophthalmology would have been greatly valued at the clinic, we had no representation of those disciplines and had allocated certain tasks with the resources at our disposal.
Study 1
METHODS
In 2021, a retrospective study was developed to evaluate the impact of the DEW Clinic telehealth model on participating students and faculty. The study was centered on the following three aims: comparing student and faculty experiences within telehealth across a spectrum of healthcare disciplines, examining the perceived benefits and challenges to providing diabetes care through telehealth, and identifying methods to improve the quality and acceptability of virtual diabetes education in underserved populations. A Qualtrics questionnaire consisting of six major questions was sent out to all participating students and faculty after each D.E.W. Clinic session from May 2021 - February 2022 (Appendix A). The questionnaire asked participants about the perceived difficulty of conducting telehealth diabetes care visits, likelihood of using telehealth for patient care in the future, and expectations vs. reality of telehealth encounters. Additional open-ended survey questions asked participants to elaborate on the benefits (Q4) and challenges (Q5) of telehealth within their specific discipline. Likert scale responses were analyzed by descriptive statistics. Qualitative responses to Q4 and Q5 were analyzed by three independent coders using an inductive approach. Once the coding was completed, a code consolidation meeting was held to establish consensus and identify broader themes.
RESULTS
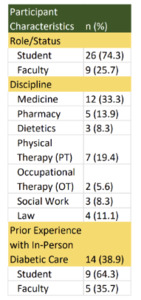
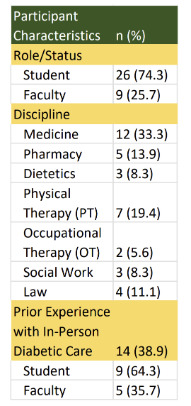
In total, 72 questionnaire responses were recorded, with a 50% completion rate. The scope of data was subsequently narrowed to 36 participant responses, which featured completion of the questionnaire in its entirety. Of these responses, 75% were from students and 25% were from faculty. Seven disciplines were represented, with Medicine (33%) and Physical Therapy (20%) comprising the largest contingents of participants (Table 2). Over ⅓ of participants had prior experience with providing in-person diabetic patient care prior to DEW Clinic participation.
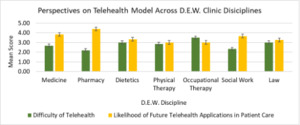
Upon analysis of the Likert scale survey items, 55.6% of respondents stated that conducting telehealth visits is “extremely easy” or “somewhat easy.” Additionally, 58.3% were “likely” or “extremely likely” to use telehealth in future practices. When results were split across disciplines, respondents from OT were the only group that found telehealth to be “somewhat difficult” on average; all other disciplines rated telehealth as “easy/neutral”. All disciplines ranged between “neutral” to “likely to use telehealth in future”.
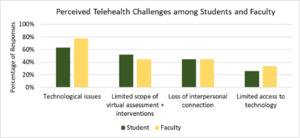
Seven themes were separately generated for both Q4 and Q5 responses in total. Thematic analysis of open-ended survey items identified four main concepts shared among all disciplines: accessibility to healthcare, improved workflow, real-time referencing, and understanding the home environment. Faculty were more likely to report “understanding home environment” as a benefit compared to students (ff = 0.4 ; fs = 0.2). Faculty were less likely to note “limited scope of assessment” as a challenge (ff = 0.4; fs = 0.5). Students were more likely to value opportunities for “real-time referencing” in a telehealth setting. (fs = 0.3; ff = 0.1).
Across multiple disciplines in D.E.W. Clinic, there was notable agreement that increased accessibility of healthcare was a primary benefit provided by the telehealth clinic model. However, there were discrepancies regarding other benefits that each discipline emphasized: 50% of respondents within Medicine, Occupational Therapy, and Law noted improved interprofessional workflow in a telehealth clinic model, while the majority in Physical Therapy (71%) felt that telehealth facilitated a better understanding of patients’ home environments.
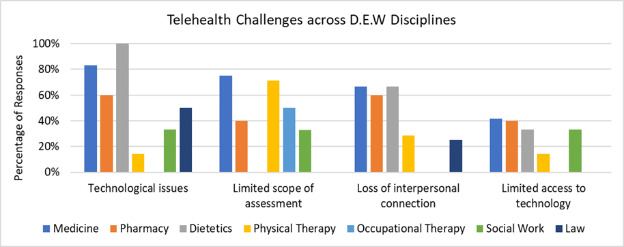
When asked about the barriers to delivering telehealth-based care, a majority of respondents in Medicine, Pharmacy, and Dietetics cited technological issues (83%, 60%, 100%) and loss of interpersonal connection (67%, 60%, 67%) as primary challenges in the D.E.W telehealth clinic model. Approximately 70-75% of respondents in Medicine and PT noted a limited scope of assessments as a significant detriment in telehealth care.
DISCUSSION
The 2021 retrospective study of the DEW Clinic telehealth model revealed that a majority of clinic participants (faculty and students) found telehealth visits easy to conduct and viewed this care model as relevant to future practices. According to participants, the telehealth model of care was reported to be beneficial for patients with diabetes, as it improved access to healthcare. Given that patients with diabetes in underserved populations experience increased morbidity and disability,4 improved access to preventive healthcare in the telehealth model could ultimately improve diabetic patient outcomes for cities such as Detroit. When further examined across each discipline, participants from OT were the only discipline that reported telehealth visits as “somewhat difficult” on average. Access to technology and functionality were more commonly identified as obstacles to delivering virtual diabetes care and education. Although it was beneficial to see patients’ home environments and help them accordingly, Physical Therapy and Occupational Therapy noted increased challenges in transitioning to the telehealth clinic model. When asked to explain, many participants from these disciplines highlighted loss of interpersonal connection and technological difficulties as drawbacks for virtual care models. Generally, most participants perceived telehealth as compromising quality care due to the inability to perform physical examinations and laboratory tests, including assessing “inaccurate edema,” measuring blood pressure, and not being able to do a proper foot exam or teach certain exercises.
Study 2
METHODS
Since past surveys were designed to evaluate the students’ and faculty’s perspectives, this survey looked at the patients’ perspectives. Once the patient met with all the disciplines, they were given a laptop to fill out a Google survey about their experience (Appendix C). The survey did not collect the patient’s name to keep it unidentifiable. The purpose was to determine if the healthcare teams were providing appropriate personalized care to the patient, and if the patient felt they received valuable information to better their health and control of their diabetes. Using a Likert scale where 1=strongly disagree and 5=strongly agree, it asked the patient a multitude of questions regarding different aspects of the clinic and their experience with it. The survey then asked the patient to choose from a list which discipline(s) helped with their needs the most, and which discipline(s) they would like to see at a follow-up visit.
RESULTS
In total, 30 responses were collected for this survey. Demographics info: Participants ranging from 18–85-year-old with type 2 diabetes; all able to speak and read English. 28 of the respondents were female, and 2 respondents were male. 71% of the patients were 65 years old or older, and 29% of the patients were younger than 65.
Analysis of the Likert scale questions revealed means ranging from 4.8 to 5, with standard deviations less than 0.8. It revealed that all the patients agreed or strongly agreed that the health professional trainees treated them with courtesy and respect, explained their health in a way that was easy to understand, talked about things to improve their health, offered valuable assistance, fostered a collaborative environment, and made the patient feel heard. 89% of patients strongly agreed that they were provided with good information about their medications. 85% of patients strongly agreed that they will likely bring up the recommendations to their healthcare provider. Among the themes being discussed in the survey, there was no significant difference between the categories, as patients agreed their experience aligned with the clinic’s goals (p-value = 0.377).
27.6% of patients felt that all the disciplines were most helpful in their visit. 6.8% of the results showed all the disciplines chosen except Law. In terms of specific disciplines, 27.5% chose Physical Therapy, 13.7% chose Dietetics, 13.7% chose Medicine, 10.3% chose Occupational Therapy, and 10.3% chose Pharmacy. When choosing which discipline the patient was interested in seeing at a follow-up visit, 7 responded that they would like to see all eight disciplines again. In terms of specific disciplines, Physical Therapy and Dietetics had the most votes (8). Pharmacy followed with 7 votes. Medicine and Occupational Therapy both had 5 votes. Social Work had 2, and Law and Public Health both had 1. None of the above was not chosen.
DISCUSSION
The results of this study highlight that patients viewed the DEW Clinic experience very positively, with Likert scale ratings averaging between 4.8 and 5.0 and minimal variability, suggesting strong consensus across participants. Patients consistently felt respected, heard, and supported, and the majority strongly agreed they received valuable information about their medications and overall health. Importantly, 85% indicated they were likely to discuss the clinic’s recommendations with their primary providers, demonstrating the clinic’s potential influence beyond the immediate visit. When identifying the most helpful disciplines, Physical Therapy, Dietetics, and Medicine were most frequently selected, while the greatest interest for follow-up visits centered on Physical Therapy, Dietetics, and Pharmacy. These findings reinforce that the interdisciplinary model is meeting patient needs and fostering engagement in ongoing diabetes management.
DEW uses a chronic care model, which is essential because it allows patients to be empowered to take care of themselves by helping them in an interdisciplinary way. It also provides the care patients are searching for, and is successful in doing so, regardless of not supplying medications or metabolic tests. They have this opportunity to meet with multiple disciplines in-person, without worrying about how they will afford the visit. It gives the patient the option to start and keep taking care of their illness.
In turn, students learn collaboration, communication, and responsibility in taking care of patients’ concerns in a timely manner. It is also an opportunity for students to practice interdisciplinary teamwork, something that other clinics typically do not provide or students do not experience until entering the workforce. Moreover, implementing a free clinic is beneficial in an urban setting, where people often lack resources. Many are not aware of community resources and self-management strategies to prevent the complications of diabetes on their overall health, making this resource extremely vital.
Study 3
METHODS
The DEW clinic was interested in learning more about student growth and learning through the unique experience that the DEW clinic offers. Beginning in 2023, a Qualtrics survey study was conducted with 12 questions. The questionnaire looked at prior discipline exposure, understanding of each discipline’s relationship to diabetes, change in outlook for each discipline, which disciplines grew in appreciation, and how much of their respective curricula prepared them to engage with the variety of disciplines available. For questions that assessed students’ perceptions and opinions, a Likert scale was used with numerical values assigned to allow for paired t-test statistical analysis. This survey was done to assess student responses; no faculty results were recorded for this study. Results were averaged and plotted using SEM error bars.
RESULTS
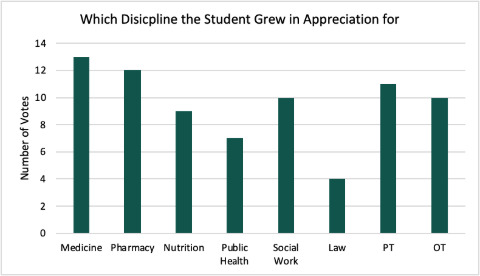
Of the 40 responses, 27 identify as women and 13 identify as male. 35 of the responses were less than 30 years old. 12 responses are from medicine, 8 from pharmacy, 6 from PT, 6 from OT, 4 from public health, 2 from social law, and 1 from nutrition and law. Regarding discipline appreciation, the results are as follows: Medicine had a value of 13, Pharmacy 12, Nutrition 9, Public Health 7, Social Work 10, Law 4, PT 11, and OT 10. The discipline appreciation results are within 1 SD from one another, except for law.
In comparing the understanding of diabetes pertaining to each discipline before and after clinic involvement, there was a statistical increase across all disciplines, with a p-value of <0.001, except Nutrition, which had a p-value of 0.046. The results are as follows: Medicine 3.82 to 4.29, Pharmacy 3.68 to 4.34, Nutrition 3.76 to 4.13, Public Health 2.63 to 3.82, Social Work 2.45 to 3.68, Law 1.68 to 2.92, PT 2.81 to 3.97, and OT 2.65 to 3.92.
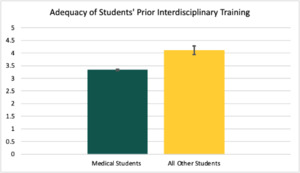
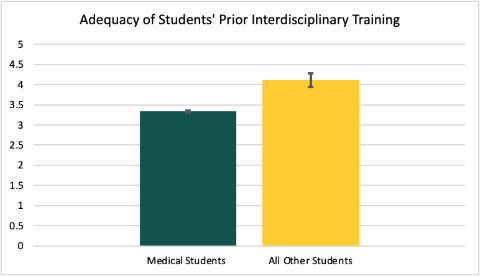
Students generally agreed that their institutions prepared them to engage with the other disciplines (value of 3.86). However, when separating medical students into a separate cohort, their average is 3.33, while the rest becomes a 4.12 with a p-value of 0.034.
DISCUSSION
The DEW clinic experience proved crucial in fostering a significant positive outlook toward all disciplines, underscoring the value of such exposure for students. Notably, there was no statistically significant difference in discipline appreciation, highlighting how each student gained some unique insight tailored to their individual need. Before volunteering, students reported a lack of understanding between diabetes and public health. Social work, law, physical therapy (PT), and occupational therapy (OT). However, their comprehension significantly improved after engaging at the clinic, suggesting a deficit in healthcare education exposure that should be integrated sooner into a student’s timeline. Furthermore, an overwhelming majority of students gained knowledge and experience concerning diabetes and its interdisciplinary relationship, advocating for the implementation of similar learning models across different disease processes to offer a more holistic approach to students. While most students felt adequately prepared by their respective educational programs to collaborate with other disciplines, medical students exhibited a decrease in their view of the interdisciplinary curriculum, raising real concerns about their exposure compared to their peers in other healthcare disciplines.5
NEXT STEPS
Future work at the DEW Clinic will focus on expanding the sample size and diversity of patient participants to better capture the needs of the Detroit community. Incorporating follow-up surveys or longitudinal studies would help determine whether patient education and recommendations provided at the clinic translate into sustained behavior change and improved health outcomes. From an educational perspective, additional evaluation methods such as direct observation, faculty assessment, or structured reflection could complement student self-report data to provide a more comprehensive view of learning. Given the differences identified in preparation across disciplines, particularly for medical students, integration of interprofessional training earlier in curricula should be explored.
Looking ahead, the DEW team hopes to expand this model to address other chronic conditions such as hypertension and COPD, further broadening its impact in the community. A hybrid model with certain disciplines participating virtually and others in person could allow for increased flexibility and efficiency. The clinic also plans to integrate residents and fellows into the interprofessional team, adding another layer of training and mentorship. Long-term tracking of patient outcomes using an electronic health system will be essential to evaluate the clinic’s sustained impact. Finally, incorporating an in-house A1c machine will allow for real-time metabolic testing and provide patients with immediate, actionable feedback during their visit.
LIMITATIONS OF THESE STUDIES
While these studies provide important insight into the impact of the DEW Clinic, several limitations should be acknowledged. First, the sample sizes were relatively small, particularly for the patient survey, which limits the generalizability of the findings. Second, the demographics of participants were not evenly distributed, as the patient group was predominantly female and older, which may not fully represent the broader Detroit population affected by diabetes. Third, all surveys were self-reported and subject to response bias, with participants potentially giving more favorable answers due to social desirability or appreciation for the clinic. In addition, the cross-sectional nature of the surveys did not allow for assessment of long-term patient outcomes or sustained student learning. Another limitation is the lack of formal language services, which prevented participation by patients with limited English proficiency, narrowing the diversity of the study group. Future studies would benefit from including interpreters or multilingual survey instruments to capture a wider range of patient voices. Finally, patient follow-up was limited, making it difficult to assess whether the recommendations provided during visits were adopted or sustained over time. Because these surveys were administered within a single institution and community setting, results may not be directly transferable to other populations or healthcare systems.
CONCLUSION
The DEW Clinic’s evolution over the past four years illustrates the adaptability and value of student-run interprofessional care models in addressing chronic disease management in underserved urban populations. The clinic’s temporary shift to telehealth during the COVID-19 pandemic revealed both the strengths and limitations of virtual care. Study 1 demonstrated that telehealth enhanced accessibility and interprofessional awareness but also highlighted critical challenges such as reduced physical exam capabilities and technological barriers. These findings directly informed the restructured in-person model introduced in 2022, which was evaluated in Study 2. Patient feedback affirmed that the redesigned clinic experience provided respectful, informative, and empowering care across multiple disciplines despite the absence of traditional diagnostic services. In addition, Study 3 emphasized the DEW Clinic’s educational value. Students across disciplines reported significant growth in understanding the holistic nature of diabetes management, while also noting varying levels of preparation in interprofessional collaboration.6 These findings underscore the need to incorporate interdisciplinary education earlier in health professions training, particularly in medical education, where the most significant gaps in exposure were identified.7
When combined, these results present DEW Clinic as a scalable, replicable model of interprofessional treatment and medical education in addition to being a local solution to diabetes inequities. Its adaptability, as evidenced by its effective use in both telehealth and face-to-face settings, makes it ideal for a variety of populations. In the future, the DEW team hopes to establish a hybrid clinic model that maintains the accessibility of telehealth while maintaining the strengths of in-person visits in terms of assessment and hands-on engagement. The DEW Clinic presents a compelling model for student-led innovation, interdisciplinary training, and patient-centered treatment as healthcare systems work to improve the outcomes of chronic diseases, especially in underprivileged areas.
Funding
The authors have no funding to report for this study.
Disclosures
The authors have no disclosures or conflicts of interest to report for this study.