INTRODUCTION
For a significant number of coronavirus disease 2019 (COVID-19) survivors, recovery from the acute phase of illness has been incomplete, leading to long-term consequences (or what is known as post-COVID-19 syndrome).1 The World Health Organization, in its study using the Delphi method in 2021, defined post-COVID-19 syndrome as a “condition [that] occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset, with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis”.1 This condition is estimated to affect 1 in 10 individuals diagnosed with COVID-19 and is associated with a constellation of physical and mental symptoms while awake and during sleep.2 One in five people, regardless of the severity of their acute infection, may exhibit symptoms for five weeks or more, while one in ten may have symptoms lasting 12 weeks or more.3 Long-term tissue damage is among the explanations for symptoms pertaining to the lungs, brain, and heart, characterized as dyspnea, cough, palpitations, chest pain, strokes, brain fog, changes in smell and taste, and mood symptoms.4,5 The objective of our retrospective survey study was to assess the chronicity of the long-term physical and mental burden on patients previously hospitalized with COVID-19.
METHODS
Patients 18-99 years of age admitted to a community hospital between May 16, 2020, and November 30, 2020, with confirmed COVID-19 were contacted by phone and/or via email. A survey with questions assessing the presence of physical and mental health symptoms before and after recovery from COVID-19 was administered verbally via phone call or electronically via an internet-based survey between December 2022 to January 2024. The analyses conducted were pre- and post-COVID-19 comparisons of anxiety, sleep quantity, sleep quality, and physical and cognitive symptoms commonly associated with post-COVID-19 syndrome. Wilcoxon Rank sum and chi-square were computed; p<.05 was considered significant. Additionally, available demographic and clinical data between respondents and non-respondents were analyzed using chi-square for presence or absence of various ordinal variable characteristics and Student’s t-test for continuous variables; p<.05 was considered significant. IRB approval was obtained for this study.
RESULTS
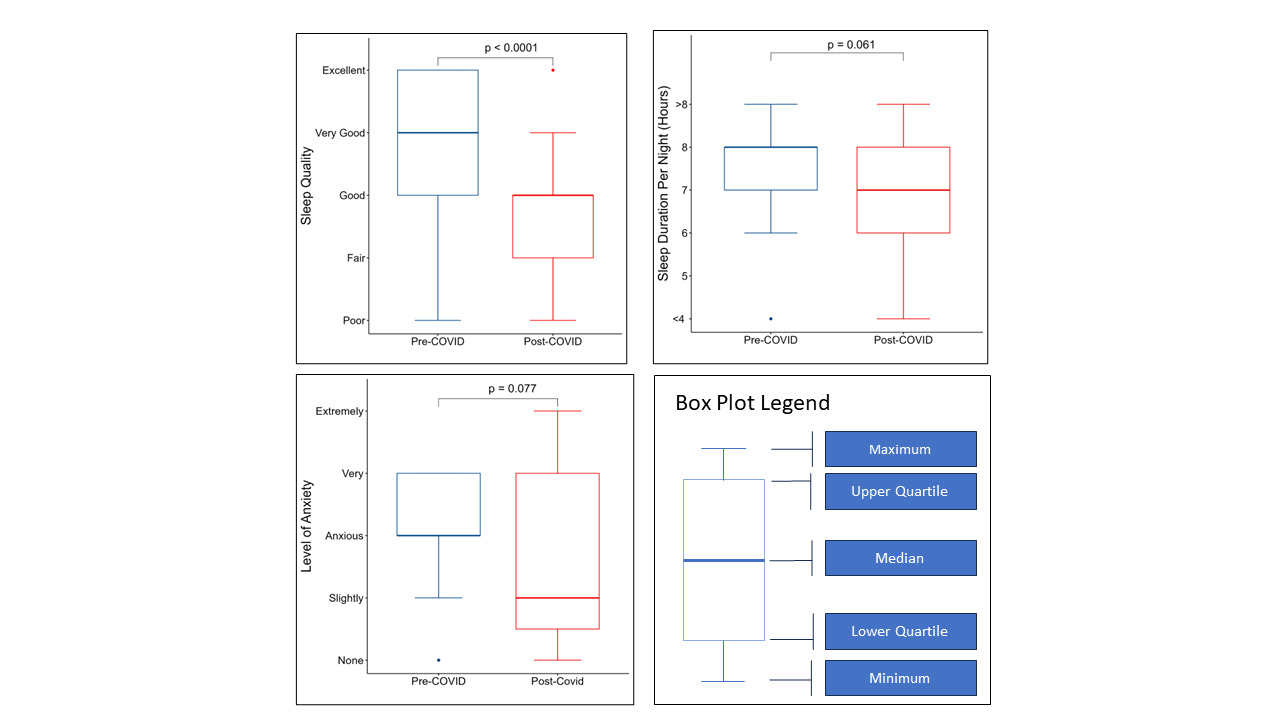
A total of 753 patients were identified for an equivocal two-wave survey6 and the present study reported on wave 2 (patients hospitalized between May 2020-November 2020). Of these patients, 17 responded to the phone survey (2.4%) and 27 responded to the email survey (3.8%) for an overall response rate of 6.2% (n=44). Respondents were asked to categorize the presence or absence of 10 symptoms based on whether the symptom was present prior to and/or following COVID-19 diagnosis. All 10 symptoms showed a significant increase following COVID-19 diagnosis (Table 1). Respondents also rated their anxiety and sleep quality using a 1-item Likert scale, and sleep quantity was reported in number of hours, both before and after COVID-19 diagnosis. Although not statistically significant, after COVID-19 diagnosis, patients reported increases in anxiety levels and sleeping fewer hours compared to before (Figure 1). However, compared to before, significantly more respondents reported decreased sleep quality after the COVID-19 diagnosis (Figure 1).
Nonresponse bias was evaluated by comparing age, self-reported race, sex, and body mass index (BMI). In 84 cases, the BMI was incorrect, and data were not available for recalculation. Results of continuous variable comparisons showed a significant difference in age between respondents and nonrespondents [t(44.5) = 3.33, p = 0.002]. However, the result of BMI comparison showed no differences between respondents and nonrespondents [t(39.4) = -0.94, p = 0.355]. Additionally, there was no statistically significant difference between gender (X2 = 2.71, p = 0.09) or race (p=0.91) and response status between respondents and non-respondents.
DISCUSSION
These findings suggest that physical complaints and sleep difficulties can persist for up to three years following a COVID-19 diagnosis and hospitalization. Results also suggest a lack of significant change in anxiety levels following COVID-19 diagnosis. Consistent with prior studies, respiratory symptoms such as cough and dyspnea were among the most frequently reported7 and may contribute to disrupted sleep—even in individuals without a history of COVID-19.8 Sleep disturbances, including insomnia, sleep-disordered breathing, and other sleep-related disorders, are commonly observed in those experiencing post-COVID-19 syndrome.9 Additionally, symptoms such as fatigue and cognitive dysfunction (“brain fog”) are frequently associated with sleep issues, with recent studies suggesting that sleep health may be a component of post-COVID-19 recovery.10 Further research is essential to better understand the clinical trajectory and optimal management strategies for individuals affected by post-COVID-19 conditions. A systematic and objective evaluation of respiratory and sleep symptoms—through modalities such as polysomnography and pulmonary function testing—is crucial for guiding treatment and monitoring long-term recovery in these patients.
CORRESPONDING AUTHOR
Laci L. Zawilinski, PhD
Department of Medical Education
Ascension Providence Hospital
16001 West 9 Mile Road
Southfield, MI 48075
Phone: 248-849-5811
Email: lzawili1@hfhs.org
FUNDING
The authors have no funding to report for this study.
DISCLOSURES
The authors have no disclosures or conflicts of interest to report for this study.
Author contributions
Data curation: Malik Abdolkarim (Lead), Akshay Bansal (Supporting). Project administration: Malik Abdolkarim (Lead). Writing – original draft: Heraa Hasnat (Lead). Methodology: Heraa Hasnat (Supporting), Akshay Bansal (Supporting), Laci L. Zawilinski (Supporting). Formal Analysis: Joseph Crutcher (Lead). Validation: Joseph Crutcher (Supporting), Jeffrey C. Flynn (Supporting). Writing – review & editing: Jeffrey C. Flynn (Supporting), Laci L. Zawilinski (Supporting), Abdulghani Sankari (Supporting). Conceptualization: Jeffrey C. Flynn (Supporting), Laci L. Zawilinski (Lead), Abdulghani Sankari (Supporting). Supervision: Laci L. Zawilinski (Supporting), Abdulghani Sankari (Supporting).